
A CANCER DIAGNOSIS and urgent need for major surgery can be devastating.
Now imagine, living in a remote community and needing to drive hundreds, if not thousands of kilometres, in wintery conditions to hear this news from a specialist.
Heavy snow and ice on British Columbia’s mountain highways lead to treacherous and unpredictable conditions during the long winter months. Even with good weather, wildlife and other hazards on remote roads and highways make driving dangerous, especially over great distances.
Using the modern practice of telemedicine, an innovative team of thoracic (chest) surgeons with UBC’s Southern Medical Program are rapidly improving access to quality medical care in small and rural BC communities.
“In one day, I can see patients in Kamloops, Prince George, Dawson Creek, and Oliver, review their medical images in real time, and determine appropriate treatment plans from our telemedicine office at the Kelowna General Hospital.”
Communicating from a distance via modern technology has already saved time, expenses and travel risk for thousands of regional patients in the Interior and Northern BC regions.
Thoracic surgery in the province is consolidated into four centres: Kelowna, Vancouver, Surrey, and Victoria.
At Kelowna General Hospital (KGH), the Interior Health Thoracic Surgical Group (IHSTG) of Drs. Shaun Deen, Michael Humer, Anand Jugnauth and Andrew Luoma serve a population of approximately one million people dispersed over 807,538 square kilometres—larger than the area of France.
Learn more about
Health Care in Real Time: Sparing travel risk and expenses
With the help of a robust and secure Skype-like videoconference technology, UBC doctors are able to seamlessly connect with patients and health-care professionals across the immense coverage area. The topography is diverse and uniquely British Columbian: a mix of mountains, valleys, forests, desert, peninsulas, inlets and islands.
About 80 per cent of IHTSG patients have cancer, most commonly in the lung or esophagus, according to Dr. Humer, Clinical Assistant Professor with the Southern Medical Program.

“In one day, I can see patients in Kamloops, Prince George, Dawson Creek, and Oliver, review their medical images in real time, and determine appropriate treatment plans from our telemedicine office at KGH,” says Dr. Humer.
“It’s often better than seeing the patient ‘in person’ as I now see them with a family member who might not have been able to travel to Kelowna for their various appointments.”
Telemedicine now represents 50 per cent of the group’s practice, enabling surgeons to connect with patients with a few clicks of a button. On average, 33 patients in 11 different communities are seen virtually each week.
The telemedicine service has grown from 320 patients in the first full year to more than 1,700 annually across the Interior and Northern Health coverage areas.
Between 2003 and 2015, the group conducted 15,073 telemedicine patient assessments from 63 different geographic locations.
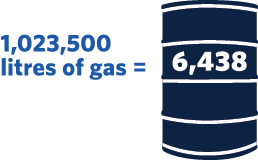
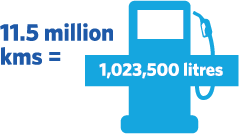
These same patients saved a total travel distance of 11.5 million kilometres, an average of 766 kms per patient. The total distance is approximately equivalent to 287 trips around the world.
Savings by the numbers

Communities and Professionals in Collaboration
Dr. Humer credits the development of the telemedicine service at KGH due in large part to the efforts of his late colleague Dr. Bill Nelems, UBC Emertius Professor.
Prior to use of telemedicine, surgeons were required to travel to rural and remote communities to provide consults and follow-ups with limited capacity. Patients would also have to travel long distances, experience lengthy wait times or, in some cases, forego care altogether.
“Dr. Nelems had many years where he drove the trip from Kelowna to Cranbrook more than five times in a year to provide distant patient assessments,” says Dr. Humer of the winding, 1,060-km round trip.

The Interior Health Thoracic Surgical Group serves a population of approximately one million people dispersed over 807,538 square kilometres—larger than the area of France.
Patients and their support network only need to come to Kelowna if they require surgery, essentially eliminating the need for travel for the initial consult and follow-up appointments. After surgery, each patient is managed in the closest “home” community in consultation with the local health-care team.
“The feedback from patients really highlights the tangible benefits of telemedicine,” says Dr. Barbara Campling, Head of Medical Oncology at BC Cancer in Kelowna and Clinical Professor with the Southern Medical Program.
“Patients, especially those who are elderly, are grateful to receive quality care while being spared the cost and stress of a multi-hour trip.”
Behind the scenes, Dr. Humer says, the commitment of Interior Health and extensive collaboration with health professionals, office staff and information technology specialists ensures the timely and reliable delivery of the vital service for people living across vast regions.
“We have removed distance from being an impediment to access to care for our patients.”