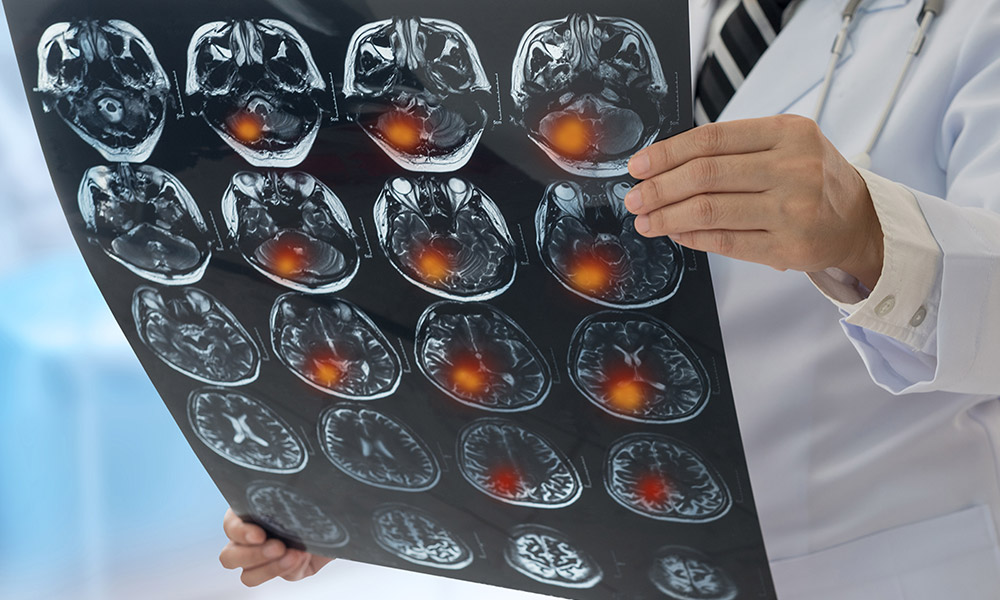
Getting medical help as quickly as possible is vital for stroke patients. A UBC Okanagan researcher uses mathematical modelling to investigate pre-hospital patient transfer policies.
Minutes matter when a stroke patient is being rushed to hospital—any delay in care can impact that person’s chance of survival and recovery.
Knowing how vital every second is for these patients, UBC Okanagan’s Dr. Amir Ardestani-Jaafari and Dr. Beste Kucukyazici from Michigan State University have analyzed transportation procedures and triage protocols to ensure stroke patients get the right level of care at the right time. Dr. Ardestani-Jaafari is an Assistant Professor in UBCO’s Faculty of Management and he specializes in health-care operations and logistics.
“Strokes, which are an attack on the brain, are a time-sensitive medical condition with only a short window available to administer therapeutic interventions,” says Dr. Ardestani-Jaafari. “Currently, patients are transported to the nearest stroke centre, following specific protocols. Yet, these protocols do not consider many factors, including the spatial variation in population density, the stroke’s severity, the time since stroke onset and the congestion level at the receiving stroke centre.”
His research, published recently in Management Science, presents a modelling framework that generates the optimal primary transport destinations for suspected acute stroke patients through an optimization model. The work also evaluates the impact of these destination decisions on patient outcomes and compares the performance of alternative policies through a simulation model.
“In our paper, we model the flow of patients in pre-hospital as well as hospital care and we examine the interactions between these two components of the stroke care continuum,” says Dr. Ardestani-Jaafari. “To be more specific, we investigate the impact of pre-hospital patient transfer policies on stroke unit congestion.”
Dr. Ardestani-Jaafari’s methodology uses mathematical modelling, including data analytics, along with discrete-event simulation, predictive and prescriptive analytics, to first understand why there is a problem in stroke transport in any urban city and what is the magnitude of the problem.
Recent medical advancements include the development of a new stroke treatment called endovascular therapy (EVT) for acute patients with a large vessel occlusion, explains Dr. Ardestani-Jaafari. Patients with this type of stroke, which is quite common, can have more complications and poor short- and long-term outcomes, he explains.
However, an EVT can remove the clot by sending a catheter to the blocked blood vessel in the brain and this can improve health outcomes.
But an EVT must be conducted in a matter of hours, meaning the patient must get to the right level of care as quickly as possible. When a destination hospital is fully congested, a patient might have to wait for admission and this wait for emergency care can have a negative impact including mortality and a person’s ability to function as they recover.
Dr. Ardestani-Jaafari’s modelling looks at whether it’s best to send a patient to a specialized stroke care facility, which may be a longer journey, instead of the closest emergency room. Getting to an emergency room that is backlogged and can’t take a patient, or cannot perform an EVT, could prove disastrous for the patient, he adds.
“The aim of this research is to find the connection and provide a solution between the delay of pre-hospital care and in boarding into a care unit,” he says. “We want to prevent any delay with the goal to improve the patient functionality at the time of discharge. This could help the patient’s recovery and their chance of returning to society and, hopefully, their ordinary lifestyle as soon as possible.”